The Mental State Examination and Its Purpose in Psychological Medicine.
Introduction
The Mental State Examination (MSE) is a tool used in psychology, psychiatry, psychological medicine or whenever it is deemed necessary and useful. It is quick, easy-to-use and is a structured method to describe, assess and observe your patient psychological functioning and mental state.
At the end of the MSE, you should have a relatively detailed description of key aspects of your patient mental state which should be written in a concise and paragraph like manner. It should be mentioned that an MSE should be made every time the patient comes and see the consultant/clinician. This is particularly useful as a history of MSE can then be made and compared to one another. By doing so, we can notice if things are improving or declining as a whole or in each segment of the MSE.
The MSE works hand in hand with the 4P factor model formulation; hence if you do both, you would a get a clear picture of your patient’s past and current life. This would allow the clinician to make a sound diagnosis, follow-ups, formulations and patient management for recovery. This includes the best course of action such as which therapy is needed, if medication needs to be started, if there is a need for referrals to certain support groups or specialists and so on. In a way, the MSE is the physical examination of the mind and is very useful, be sure to study and practise for a seamless and successful consultation!
Check out my other blog in psychology relating to the MSE formulation “The 4P Factor Model and Its Purpose in Psychological Medicine”.
Art illustration by Famous When Dead from the creator strange and intriguing artworks. The artwork is heavily influenced by popular culture, past and present and constantly on the lookout for fresh ideas.
How to use the ASEPTIC technique in the MSE
The Mental State Examination (MSE) is organised and structured by using the ASEPTIC acronym. By using the acronym, you know that you are covering all the most important aspects in an orderly and systematic fashion. There is a lot to remember and it will get easier over time as you will be practising more often. I have added as much as I could in terms of description in each segment. You don’t have to remember them all but do understand the general idea per section and bear in mind to do the MSE every time you see your patient.
Note: make a mental note of your patient’s age and development level or if they have any syndromes that affect their cognition and intelligence. If there is anything on suicide or homicidal ideation in children or adolescent, they must be referred immediately for their safety.
ASEPTIC
(A)ppearance and Behaviour
How does the patient look? Observe the patient’s behaviour.
General appearance: ethnicity, gender, age, BMI prediction, any syndrome present?
Note what the patient is doing during the examination, look at non-verbal communication
Look for cues of lifestyle, daily living skills, quality of self-care
Clothing and hairstyle. If he is a male - how is the shave? If she is a female, how is the makeup?
Groomed or dishevelled
Hygiene and cleanliness
Gait, posture, general body habitus, any abnormal movement?
Psychomotor activity (relates to mental activity): normal, reduce and excessive
Attitude towards the examiner: submissive/withdrawn, cooperative or evasive, overfamiliar/seductive, defiant/hostile, eager to please, fearful
Facial expression and body language
Eye contact: good, bad, avoidant, piercing, unblinking
Have you ever seen Dr Hannibal Lecter (by Anthony Hopkins) in The Silence of the Lambs? Here he is represented on the image on the left hand side. Recall the first time the movie introduces him when he is standing in his cell, what was your first impression? Did you know that he never blinks (or at least very little compared to a normal person) during the conversation? He also gives this weird ‘off-putting’ vibe due to his body language, why and how is that?
(S)peech: Rate, Tone, Volume and Quality
How is the patient speaking?
Rate/speed: rapid, pressured, slow, mute, interruptible
Tone: monotone or sing-song like, low to high, shaking and quivering tone?
Volume: loud, yelling, quiet, whispering, inaudible
Quantity: monosyllabic or verbose, minimal to excessive, repetitive
Quality: clear pronunciation or slurred, articulation
Other: accents; response only to questions or provides heaps of information
Note: notice if any diseases would affect speech such as dementia, trauma, cancer, muscle weakness, brain injuries, speech disorder, degenerative diseases, hearing loss, autism and so on. It would be slightly embarrassing if the reason for a change in the patient’s speech was due to another disorder other than psychological.
(E)motion: Mood and Affect
How would the patient describe their predominant emotions over days/weeks? Observe their current emotional state.
Mood and affect are both involved with emotions, but they are different from one another. Mood describes the emotion of the patient over a period of time whereas affect describes the immediate expression of a certain emotion that you observed during the consultation. Mood causes a person to see the world differently, for example, think of someone who is depressed for a long time as he or she may see the world gloomy, sad and maybe with a bit of pessimism.
Mood:
You have to question your patient about their feelings they have had lately and get an insight into their emotional history.
How have you been lately?
How are you currently feeling? How is your mood?
Over the past days or weeks have you been feeling depressed, elevated, anxious, apathetic?
Mood state may be:
Euthymic
Dysthymic/down/depressed
Hyperthymic/high/elevated
Angry/irritable
Anxious, apathetic
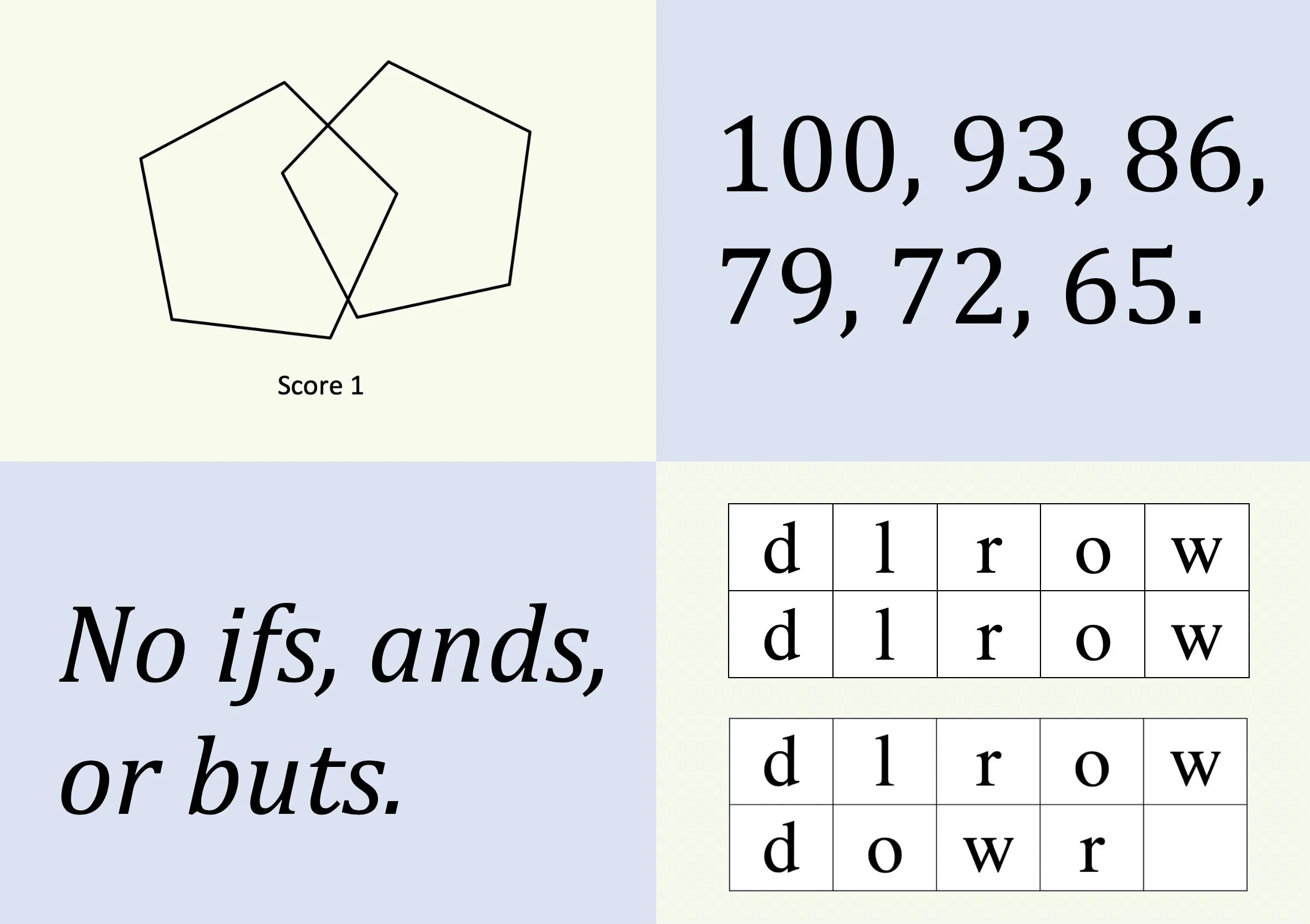
Using a scale from 0-10 may be appropriate to gauge the mood of a patient. Where 0 is extremely sad with possible wanting to end their life to 10 which is extremely happy.
Affect:
The overall emotional tone must be objectively observed during the consultation and always compare if the emotion is appropriate to the situation. For example, they may be laughing which is normal but if they were laughing hysterically about a family member or a pet being dead then the situation may not be so normal.
Reactive - appropriate to the context, no abnormality found
Quality: euthymic, elevated, depressed
Range: full (normal), constricted/restricted to broad
Stability and fluctuation: fixed or labile (easily altered)
Intensity: normal, flat, dampened, intense
Appropriateness and congruency: does it match the mood? Is the mood appropriate to the situation, i.e. the patient’s family member has passed away and they feel sad. Incongruent would be patient mood does not match the situation.
(P)erception
Is the patient interpretation of their surroundings misinterpreted?
Illusions: distortion of perception
Hallucinations: olfactory, visual, auditory
Altered bodily experience: depersonalisation, derealisation
A hallucination is when the patient perceives and believe something is real even though there was no external stimulation. For example: hearing something but there was no sound present.
An illusion is when a person mistakes or misinterpret a perception such as a chair full of clothes at night may look like a person is sitting on it — in other words, mistaking one object for another.
Note: the most common hallucination is auditory such as hearing voices (especially in schizophrenia). Hence, during the consultation, there needs to be an assessment of the quality of the voices. For example: if the patient can control the voices, if it is internal or external, if the voices are commenting on everything or gives orders to do certain acts (very important), if the patient is aware that the voices are real or not such as if they are aware they are hallucinating and understand that it is not real (pseudo-hallucination).
Questions to ask could be:
Are you hearing, seeing, smelling and tasting things that others can’t hear, see, smell or taste?
Have you seen, smelt, heard or taste anything that is not really there?
At the time did you think it was real?
Currently, do you still think it was real?
Do you ever feel what is around you is not real?
Do you feel you are not real?
(T)houghts: Form, Content and Possession
What is the patient thinking about? Observe their logical thinking.
Thought form represents how someone is expressing their thoughts in their speech such as their speed, their flow of ideas and if their thoughts are disjointed, illogical or repetitive. In other words, it describes the rate of thoughts, how they flow and how they are connected. Thought content relates to the actual thought being described or the theme that occupies their thoughts. Thought possession involves a patient experiencing their thought being removed, implanted or heard from other people. This is generally hand in hand with paranoia and conspiracy theories about the government.
Thought form:
Speed:
slowed/accelerated/racing
Flow:
Thought blocking: interrupted thoughts
Flight of ideas: quickly moving from one idea to another
Word salad: random words being spoken
Preservation: repetition phrases, words or ideas
Circumstantial: eventually gets to the point after an unnecessary amount of detail
Tangential: moving from thought to thoughts that are related but does not get to the point
Loose: illogical relation of thoughts between unrelated topic
Normal flow: logical, linear, goal orientated
Abnormal flow: disordered, circumstantial, tangential, incoherent, derailment, looseness of associations
Thought content:
Delusion: grandiose, somatic, bizarre, paranoia
Suicide ideation
Homicidal ideation
Obsession: the patient is obsessed with an idea and cannot get it out of their head
Overvalued ideas: can be described in patients with anorexia nervosa where they have to lose weight or count every food item that has been eaten
Phobias: irrational fear of something
Magical thinking
Thought possession:
Thought insertion: the patient believes thoughts have been inserted into their heads
Thought withdrawal: the patient believes thoughts have been extracted from their heads
Thought broadcasting: the patient believes thoughts are being heard from other people
Questions to ask could be:
Do you feel people can hear what you are thinking?
Do you think people have put ideas in your head?
Do you feel that people have removed or erased memories from your mind?
(I)nsight and Judgement
How aware is the patient about their condition/situation?
Insight is about how aware the patient is about their illness, the situation they are in and do they understand it. It is also about the acceptance of their problem and if they accept the needed help or treatment. Does the patient want help or do they know what is the cause of their problem or do they recognise what they are experiencing is abnormal? Judgement is about their problem solving and to be able to respond correctly and rationally to a situation. It is also about making proper decisions and anticipates the consequences of their behaviour.
Insight:
Assuming the patient had difficulties or illnesses, how do they perceive this and do they acknowledge?
Good/intact insight: the patient is understanding what is happening, accepts it and seek treatment to get better. The patient understands all the factors that have led to this situation and wants to have a healthier outcome.
Partial insight: the patient understands there is a problem and acknowledges it but decides not to seek help or treatment.
Poor insight: the patient does acknowledge they are ill, does not accept the situation, may shift the blame on others to why this is happening and does not want to seek help or treatment. They may blame external locus and that everything is happening because it is out of their control.
Judgement:
Present a case and see their approach on the situation, for example, if you smell smoke in the house what is your next course of action?
Can the patient make reasonable decisions
Intact, fair or impaired judgement
(C)ognition
Is the patient orientated? Test their memory and observe their attention.
Ability to process information and memory (short and long term). Is the patient able to demonstrate good problem solving and reasoning, knows the place and time and is the patient alert and orientated?
Level of consciousness: alert, lethargic, stuporous, confused
Orientation in 3 different areas: name, time and place
Attention: good or poor, how well can they focus, do they need redirection or repetition
Memory: immediate, short and long term recollection and how well can they remember
Intelligence: based on your observation, does the patient appears to be below average, average, above average?
Mini Mental State Examination (MMSE) can be used to see if there is any cognitive impairment or the Addenbrooke’s Cognitive Examination - ACE III can also be used.
Before and after the ASEPTIC
Before:
Introduction: state name, position, ask for patient’s preferred name.
Wash hands.
Explain what is the MSE and obtain consent.
Any questions from the patient.
After:
Thank the patient.
Conclude and summarise the findings.
Any questions from the patient.
Wash your hands.
Thank you and goodbye.
Case study: John Doe
Use the ASEPTIC formula and delegate this case study to each segment. This is a fictitious case as I tried to add something to each segment just to demonstrate how an MSE would look like.
Mr Doe, 55 years old, arrives at your practice and is concerned. He is about 175 cm and weighs 90 kilograms, and he is limping from his right leg as he mentions that it is still painful from the work accident. He looks well, neat and tidy and has a nice clean shave.
During the consultation, he would stand up and sit down several times whilst clutching his fists in anger. Most of the consultation he spoke calmly, clearly and had good eye contact when doesn’t talk about his work. Every now and then, his tone and volume would fluctuate. His thoughts were logical and made sense; however, he did repeat his idea of suing the firm he worked for a few times. John denies any suicidal feelings, but he did mention that he feels not worthwhile and felt isolated in the workplace as he had to leave his old workplace to a new one due to an accident. He feels that the accident at his previous workplace was entirely the officer in charge’s fault.
John denies any hallucination or illusions. After a large number of uneventful details, he finally confesses that he has been a problematic employee and colleague. John feels hopeless as he feels that his superannuation will not be able to sustain himself and his wife when he retires. He speaks a lot about the failure of his retirement funds which has been making him feel ‘low’ for the past year. Whilst asking about his family relation, he mentions that he has not been the best farther and sometimes finds himself crying at the thought as he regrets some of his actions.
Upon asking where he is, his full name and surname and what day/month it was, John managed to answer all the questions successfully and seemed to be alert and orientated. John does display poor concentration, and his processing was slow. When asked to remember a few things, he seemed to struggle to remember certain events. He says he usually remembers these events quite well. He admits that it is essential to see a GP and speak about his issues but does not take any responsibility for the problems happening in his life.
Write down ASEPTIC on a piece of paper and try to remember what each letter stands for. When you are doing this for the first time just remember the title and try in figuring out which description would go into which segments. Did you manage to fill all the segments correctly? Was there any overlapping description that you felt should go into more than one segment? As you practice more often, you will start to learn more about each segment and their description. To this date, I have yet to practice on a real patient as I believe it can be quite difficult to ask the right questions at the right time and manage to write everything down. One thing for sure is that my psychology rotation in 5th year is definitely going to be interesting, exciting and challenging!
Conclusion
Remember the ASEPTIC is a structured formula to create a quick and thorough detail of your patient’s mental state. It should be intuitive and flow logically. Technically a presenting case should be way longer than this, and the Mental State Examination (MSE) is pretty much the size of the case above with all sections put together. As I mentioned before, the MSE should be done every time you see your patient so that you can compare any progress, whether positive or negative. That is not to say the MSE has to be very detailed when the patient is coming in for a sore throat. However, during your consultation, you can always be aware of the basics and make some notes; for example, how was the appearance of the patient? His or her speech? Did he/she seem orientated? Were his/her thoughts flowing logically? How is he/she feeling? Unless the patient is coming in for a psychological consultation then the MSE can be a lot more detailed and thorough as you can use extra tests such as the Mini Mental State Examination.
Now utilise the 4P factor model formulation to get an even better outlook on your patient’s life as it describes what happened previously (predisposing), what is happening now (precipitating), what is reoccurring (perpetuating) and if the patient has any protective factor. I shall cover the 4P factor model formulation in the next upcoming blog.
At the end of the Mental State Examination, the clinician would be able to make a sound diagnosis, suggest follow-ups if needed, prepare sound formulations and/or patient management for a successful recovery. This would include the best course of action such as which therapy is needed, if medication needs to be started, if there is a need for referrals to certain support groups or specialist and so on.
Published 30th November 2019. Last reviewed 30th September 2022.
Reference
H. Combs. Mental Status Exam. University of Washington website. https://depts.washington.edu/psyclerk/secure/mentalstatusexam.pdf. Published Apr 23rd, 2008. Accessed November 25, 2019.
Lewis Potter. Mental State Examination (MSE) – OSCE Guide. Geeky Medics. https://geekymedics.com/mental-state-examination/. Published 2018. Accessed November 25, 2019.
Susan Ayers, Richard de Visser. Psychology for Medicine. 1st ed. London: SAGE Publication Ltd; 2011. ISBN: 978-1-4129-4690-2.
T. Abecassis, D. Aggarwal, M. St-Jean, E. Wooltorton, F. Motamedi, M. Cheng. Mental Status Examination (MSE). eMental Health Primary Care. https://primarycare.ementalhealth.ca/index.php?m=fpArticle&ID=26974. Revised Oct 4th, 2019. Accessed November 25, 2019.
The Royal Children’s Hospital Melbourne. Mental state examination. The Royal Children’s Hospital Melbourne website. https://www.rch.org.au/clinicalguide/guideline_index/Mental_state_examination/. Updated November, 2018. Accessed November 25, 2019.
University College Dublin. Mental State Examination. University College Dublin website. www.ucd.ie/psycheducation/samplecontent/Taking_Case_Histories/data/downloads/mentalstateexamination.pdf. Modified 2012. Accessed November 25, 2019.
University of New South Wales. Comorbidity Guidelines Training Program: Session Three - Handouts Assessment of Mental State. University of New South Wales website. https://ndarc.med.unsw.edu.au/sites/default/files/ndarc/resources/Session%203%20Handouts.pdf. Accessed November 25, 2019.